Inside the Medical Diagnostic Assembly Machine: How Precision Engineering Improves Accuracy
AUGUST 28, 2025
Medical diagnostic assembly machines are automated production systems that build high-precision diagnostic devices with repeatable accuracy. In healthcare, small misalignments can skew signals or flow paths, so design and assembly must hold tight tolerances to keep readings reliable. Automation, vision inspection, and traceable quality records help manufacturers meet demanding requirements such as ISO 13485(https://www.iso.org/standard/59752.html) quality management for medical devices.
This article explains what these machines do, the modules that keep performance consistent, and how precision engineering raises accuracy for products like glucose meters, cholesterol testers, and multi-parameter monitors. We will also touch on standards for glucose meter accuracy.
This article explains what these machines do, the modules that keep performance consistent, and how precision engineering raises accuracy for products like glucose meters, cholesterol testers, and multi-parameter monitors. We will also touch on standards for glucose meter accuracy.
What Is a Medical Diagnostic Assembly Machine?
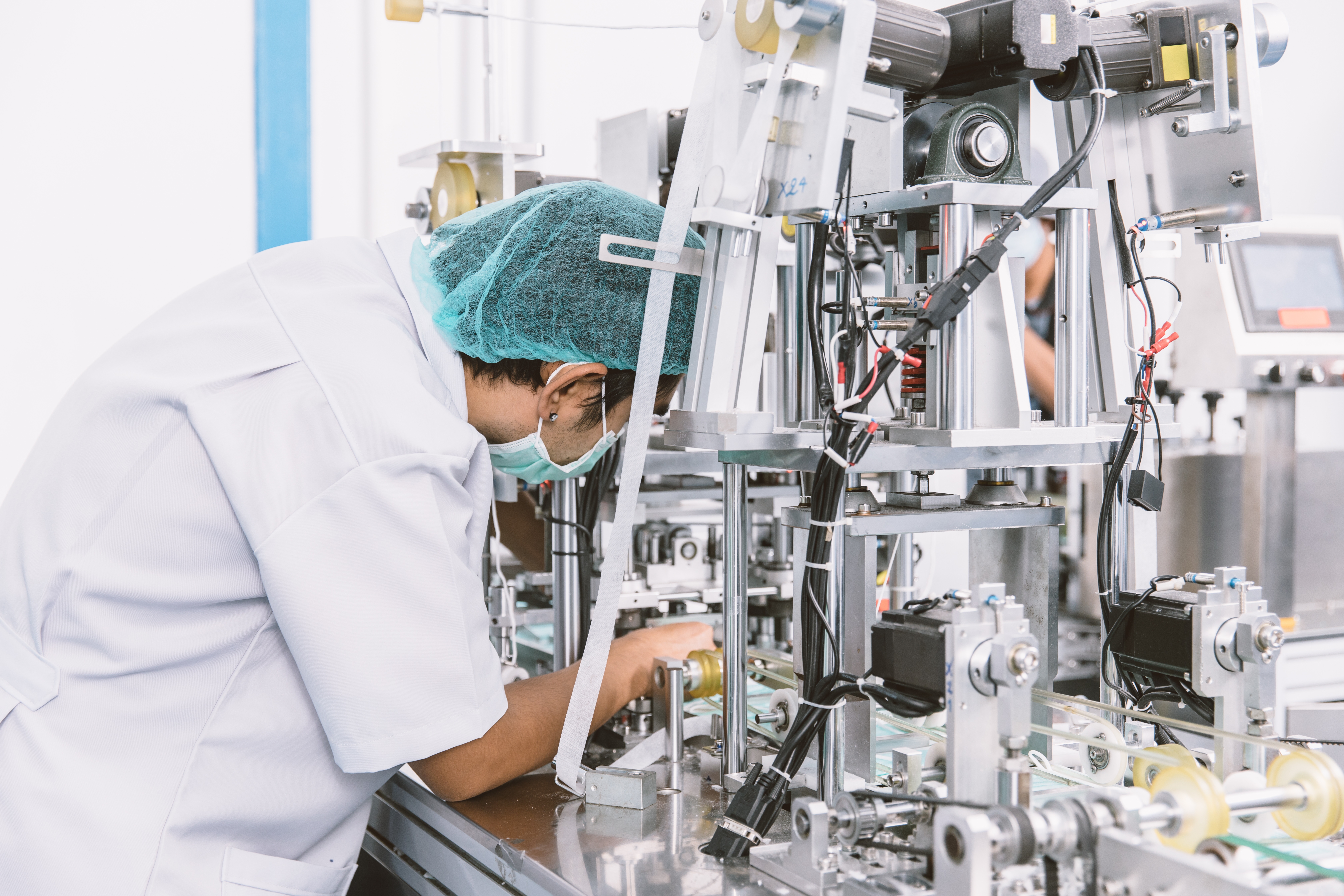
A medical diagnostic assembly machine refers to an automated system within the manufacturing line that constructs diagnostic instruments from their individual parts. This equipment takes over tasks such as inserting sensors, placing microchips, and bonding housing components in a cleanroom environment to guarantee precision and uniformity.
Common diagnostic tools assembled by these machines include:
●Glucose meters and lateral flow test strips
●Cholesterol or multi‑parameter monitors
●Test kit cartridges, microfluidic chips, biosensors, and cassettes
Assembly accuracy directly links to measurement accuracy in the end device. When delicate parts such as biosensor films or reagent membranes are misaligned even by microns, it can lead to inconsistent sample contact, optical drift, or electrical variances. High-precision automated assembly ensures each device performs within required tolerances, leading to reliable output. Consistent placement and bonding also support effective calibration and reduce failure rates under regulatory audit or real-world use.
Common diagnostic tools assembled by these machines include:
●Glucose meters and lateral flow test strips
●Cholesterol or multi‑parameter monitors
●Test kit cartridges, microfluidic chips, biosensors, and cassettes
Assembly accuracy directly links to measurement accuracy in the end device. When delicate parts such as biosensor films or reagent membranes are misaligned even by microns, it can lead to inconsistent sample contact, optical drift, or electrical variances. High-precision automated assembly ensures each device performs within required tolerances, leading to reliable output. Consistent placement and bonding also support effective calibration and reduce failure rates under regulatory audit or real-world use.
Key Components and Functions
This section outlines the critical systems within a medical diagnostic assembly machine, each vital for achieving precision, repeatability, and compliance.
1. Automated Assembly Modules
Automated assembly modules perform precise placement of delicate parts such as biosensors(https://pmc.ncbi.nlm.nih.gov/articles/PMC4986445/), microchips(https://www.asml.com/technology/all-about-microchips/microchip-basics), reagent films, and test strips. These sub-systems, similar to surface-mount pick-and-place machines used in electronics production, use robotic heads (often gantry-based) with suction nozzles and integrated cameras. The cameras align components, correct positional and rotational errors, and place each element with accuracy often below half a millimeter. In high-volume operations, such repeatable precision ensures uniform device behavior across batches.
2. Calibration and Testing Units
Integrated inline testing units evaluate each assembled device before packaging. These systems, often referred to as Automatic Test Equipment (ATE), interface with the assembled device called the Device Under Test (DUT) and run functional checks such as electrical responses, sensor outputs, and calibration accuracy.
For blood glucose meters, inline calibration verifies compliance with ISO 15197:2013(https://www.iso.org/standard/54976.html) standards, ensuring 95 % of results fall within ± 15 mg/dL below 100 mg/dL or ± 15 % at or above 100 mg/dL. This ensures each unit meets global performance expectations before release.
3. Material Handling Systems
Material handling systems manage the movement of components from feeders to assembly areas. These systems must be non-invasive to protect fragile and sterile parts. Common mechanisms include tape-and-reel feeders, trays, and robotic handlers that minimize contact, static, and contamination risks. This is especially important for biocompatible materials and microfluidic elements commonly used in diagnostic devices.
4. Quality Control Integration
Visual inspection systems detect defects in real time using machine-vision techniques. Automated Optical Inspection (AOI)(https://en.wikipedia.org/wiki/Automated_optical_inspection) uses cameras to scan components for missing parts, misalignments, solder defects, and orientation flaws.
For internal defects, Automated X-ray Inspection (AXI)(https://en.wikipedia.org/wiki/Automated_X-ray_inspection) may be employed to verify component alignment and detect hidden faults. Quality control software immediately rejects non-conforming units and logs results for traceability vital for audits, recalls, and regulatory compliance.
5. System Validation and Regulatory Traceability
All modules must undergo installation qualification (IQ) and operational qualification (OQ) within the manufacturer’s facility. These tests verify that machines are built and operate according to specified requirements. If changes occur, such as reconfiguring modules or switching components, the assembly process may require revalidation, including developing and executing test protocols, risk assessments, and documentation for repeated approval.
1. Automated Assembly Modules
Automated assembly modules perform precise placement of delicate parts such as biosensors(https://pmc.ncbi.nlm.nih.gov/articles/PMC4986445/), microchips(https://www.asml.com/technology/all-about-microchips/microchip-basics), reagent films, and test strips. These sub-systems, similar to surface-mount pick-and-place machines used in electronics production, use robotic heads (often gantry-based) with suction nozzles and integrated cameras. The cameras align components, correct positional and rotational errors, and place each element with accuracy often below half a millimeter. In high-volume operations, such repeatable precision ensures uniform device behavior across batches.
2. Calibration and Testing Units
Integrated inline testing units evaluate each assembled device before packaging. These systems, often referred to as Automatic Test Equipment (ATE), interface with the assembled device called the Device Under Test (DUT) and run functional checks such as electrical responses, sensor outputs, and calibration accuracy.
For blood glucose meters, inline calibration verifies compliance with ISO 15197:2013(https://www.iso.org/standard/54976.html) standards, ensuring 95 % of results fall within ± 15 mg/dL below 100 mg/dL or ± 15 % at or above 100 mg/dL. This ensures each unit meets global performance expectations before release.
3. Material Handling Systems
Material handling systems manage the movement of components from feeders to assembly areas. These systems must be non-invasive to protect fragile and sterile parts. Common mechanisms include tape-and-reel feeders, trays, and robotic handlers that minimize contact, static, and contamination risks. This is especially important for biocompatible materials and microfluidic elements commonly used in diagnostic devices.
4. Quality Control Integration
Visual inspection systems detect defects in real time using machine-vision techniques. Automated Optical Inspection (AOI)(https://en.wikipedia.org/wiki/Automated_optical_inspection) uses cameras to scan components for missing parts, misalignments, solder defects, and orientation flaws.
For internal defects, Automated X-ray Inspection (AXI)(https://en.wikipedia.org/wiki/Automated_X-ray_inspection) may be employed to verify component alignment and detect hidden faults. Quality control software immediately rejects non-conforming units and logs results for traceability vital for audits, recalls, and regulatory compliance.
5. System Validation and Regulatory Traceability
All modules must undergo installation qualification (IQ) and operational qualification (OQ) within the manufacturer’s facility. These tests verify that machines are built and operate according to specified requirements. If changes occur, such as reconfiguring modules or switching components, the assembly process may require revalidation, including developing and executing test protocols, risk assessments, and documentation for repeated approval.
Regulatory Requirements and Testing Standards
The path from concept to market for medical diagnostic devices involves extensive regulatory oversight that directly drives the need for precision assembly. Understanding these requirements helps explain why automated systems with micron-level accuracy aren’t just desirable—they’re essential for regulatory compliance and commercial viability.
The Rigorous Testing and Certification Process
Class II medical devices like blood glucose monitors must navigate a complex regulatory pathway before reaching patients. The testing requirements are comprehensive and unforgiving, demanding consistent performance across multiple validation phases:
Safety and Performance Testing encompasses several critical areas. Electromagnetic Compatibility (EMC) testing ensures devices function properly in the presence of electromagnetic interference from other medical equipment, mobile phones, and hospital systems. Biocompatibility assessments verify that materials in direct or indirect contact with patients won’t cause adverse reactions or toxicity.
Analytical Performance Validation includes accuracy, repeatability, reproducibility, and linearity testing across the device’s measurement range. Limits of Detection (LoD) and Limits of Quantification (LoQ) must be established to define the smallest measurable concentrations the device can reliably detect and quantify.
Interference Testing evaluates how common substances affect measurement accuracy. Devices must demonstrate reliable performance despite the presence of vitamin C, uric acid, cholesterol, and various medications that patients commonly take. Even minor assembly variations can create interference susceptibility that leads to regulatory rejection.
Clinical Validation requires trials involving ≥100 human subjects to demonstrate real-world performance against reference laboratory methods. These studies validate that the assembled devices perform consistently across diverse patient populations and usage conditions.
Economic and Timeline Implications
The regulatory pathway from R&D to market launch typically spans 3–5 years with development costs ranging from $500K to $1M per device type. These figures underscore why precision assembly becomes economically critical; any manufacturing inconsistency that leads to regulatory delays or rejections can multiply these already substantial investments.
Stricter regulations continue to raise both costs and standards, making first-time regulatory approval increasingly important. Devices that fail initial submissions face additional testing cycles, extended timelines, and compounded development costs. This regulatory reality drives manufacturers toward automated assembly systems that can demonstrate consistent, documentable performance across every unit produced.
The combination of rigorous testing requirements and substantial development investments makes precision assembly not just a manufacturing preference, but a business necessity for successful medical device commercialization.
The Rigorous Testing and Certification Process
Class II medical devices like blood glucose monitors must navigate a complex regulatory pathway before reaching patients. The testing requirements are comprehensive and unforgiving, demanding consistent performance across multiple validation phases:
Safety and Performance Testing encompasses several critical areas. Electromagnetic Compatibility (EMC) testing ensures devices function properly in the presence of electromagnetic interference from other medical equipment, mobile phones, and hospital systems. Biocompatibility assessments verify that materials in direct or indirect contact with patients won’t cause adverse reactions or toxicity.
Analytical Performance Validation includes accuracy, repeatability, reproducibility, and linearity testing across the device’s measurement range. Limits of Detection (LoD) and Limits of Quantification (LoQ) must be established to define the smallest measurable concentrations the device can reliably detect and quantify.
Interference Testing evaluates how common substances affect measurement accuracy. Devices must demonstrate reliable performance despite the presence of vitamin C, uric acid, cholesterol, and various medications that patients commonly take. Even minor assembly variations can create interference susceptibility that leads to regulatory rejection.
Clinical Validation requires trials involving ≥100 human subjects to demonstrate real-world performance against reference laboratory methods. These studies validate that the assembled devices perform consistently across diverse patient populations and usage conditions.
Economic and Timeline Implications
The regulatory pathway from R&D to market launch typically spans 3–5 years with development costs ranging from $500K to $1M per device type. These figures underscore why precision assembly becomes economically critical; any manufacturing inconsistency that leads to regulatory delays or rejections can multiply these already substantial investments.
Stricter regulations continue to raise both costs and standards, making first-time regulatory approval increasingly important. Devices that fail initial submissions face additional testing cycles, extended timelines, and compounded development costs. This regulatory reality drives manufacturers toward automated assembly systems that can demonstrate consistent, documentable performance across every unit produced.
The combination of rigorous testing requirements and substantial development investments makes precision assembly not just a manufacturing preference, but a business necessity for successful medical device commercialization.
How Precision Engineering Improves Accuracy?

Precision engineering in medical diagnostic assembly significantly increases the reliability and longevity of devices. This section breaks down how specific factors contribute to enhanced measurement accuracy and consistent performance.
1. Micron-Level Tolerances
Modern assembly equipment operates with micron-level precision, meaning placement errors are kept within micrometers. This level of accuracy is vital for medical devices where optical alignment, electrical paths, or fluid channels must be exact. Variances beyond a micron can cause functional defects or misreadings in diagnostic instruments.
Precision manufacturing drives consistent high-quality output while reducing scrap and rework, especially important as tolerances tighten below one millimeter. In high-speed production, even a scrap rate of 0.5% can lead to substantial costs and delays.
2. Sensor Positioning Accuracy
Sensor placement must be exact to maintain calibration integrity and device lifespan. Misalignment, even slight, can cause calibration drift, reduce sensitivity, increase noise in readings, or shorten sensor lifespan due to uneven stress.
Assembly machines with precision positioning help each sensor, biochemical, optical, or electrical, to maintain its intended orientation and contact interface, ensuring reliability over time. While specific clinical examples are limited, sensor drift is widely recognized as a critical issue in device performance.
3. Minimized Human Error
Manual assembly introduces variability differences in force, alignment, or technique can lead to inconsistent outcomes. Automation removes these variables by using programmed motion control and feedback systems. The result is stable throughput and uniform device quality.
Particularly in medical manufacturing, where traceability and repeatability are non‑negotiable, automation helps maintain high standards across every batch without reliance on operator skill.
4. Consistent Calibration Processes
Accurate equipment measurement starts with calibration. Calibration is the practice of comparing device output against a known reference standard to adjust for errors. It’s essential in medical device manufacturing to reduce measurement uncertainty to acceptable levels and to maintain trust in results.
●Traceable Standards: Calibration often leverages standards from national metrology institutes (like NIST in the U.S.), ensuring a consistent measurement lineage.
●Regulatory Expectations: ISO 13485 mandates documented, systematic calibration of all test and measurement equipment. This forms the backbone of traceable quality management systems.
●Automation Benefits: Automated calibration systems reduce human error and improve the frequency of calibrations. They can store log files, raise alerts when devices drift, and ensure consistent measurement across the production line.
Given the complex regulatory landscape and substantial financial risks outlined above, selecting a manufacturing partner with proven precision assembly capabilities becomes critical for device developers.
The combination of rigorous testing requirements, multi-year timelines, and million-dollar development costs means that assembly inconsistencies can derail entire product launches. This reality drives companies toward established manufacturers who can demonstrate both technical precision and regulatory compliance from day one.
1. Micron-Level Tolerances
Modern assembly equipment operates with micron-level precision, meaning placement errors are kept within micrometers. This level of accuracy is vital for medical devices where optical alignment, electrical paths, or fluid channels must be exact. Variances beyond a micron can cause functional defects or misreadings in diagnostic instruments.
Precision manufacturing drives consistent high-quality output while reducing scrap and rework, especially important as tolerances tighten below one millimeter. In high-speed production, even a scrap rate of 0.5% can lead to substantial costs and delays.
2. Sensor Positioning Accuracy
Sensor placement must be exact to maintain calibration integrity and device lifespan. Misalignment, even slight, can cause calibration drift, reduce sensitivity, increase noise in readings, or shorten sensor lifespan due to uneven stress.
Assembly machines with precision positioning help each sensor, biochemical, optical, or electrical, to maintain its intended orientation and contact interface, ensuring reliability over time. While specific clinical examples are limited, sensor drift is widely recognized as a critical issue in device performance.
3. Minimized Human Error
Manual assembly introduces variability differences in force, alignment, or technique can lead to inconsistent outcomes. Automation removes these variables by using programmed motion control and feedback systems. The result is stable throughput and uniform device quality.
Particularly in medical manufacturing, where traceability and repeatability are non‑negotiable, automation helps maintain high standards across every batch without reliance on operator skill.
4. Consistent Calibration Processes
Accurate equipment measurement starts with calibration. Calibration is the practice of comparing device output against a known reference standard to adjust for errors. It’s essential in medical device manufacturing to reduce measurement uncertainty to acceptable levels and to maintain trust in results.
●Traceable Standards: Calibration often leverages standards from national metrology institutes (like NIST in the U.S.), ensuring a consistent measurement lineage.
●Regulatory Expectations: ISO 13485 mandates documented, systematic calibration of all test and measurement equipment. This forms the backbone of traceable quality management systems.
●Automation Benefits: Automated calibration systems reduce human error and improve the frequency of calibrations. They can store log files, raise alerts when devices drift, and ensure consistent measurement across the production line.
Given the complex regulatory landscape and substantial financial risks outlined above, selecting a manufacturing partner with proven precision assembly capabilities becomes critical for device developers.
The combination of rigorous testing requirements, multi-year timelines, and million-dollar development costs means that assembly inconsistencies can derail entire product launches. This reality drives companies toward established manufacturers who can demonstrate both technical precision and regulatory compliance from day one.
Bioptik’s Approach to Precision Assembly
Bioptik is a Taiwan‑based manufacturer founded in 1999, with over 26 years of experience in diagnostic device development and production. Its operations include three production facilities and R&D centers located in Miaoli (Jhunan Township), Hsinchu, and Tainan, each dedicated to specific product streams from medical reagents and diagnostic tools to skincare and bioenergy solutions.
All facilities are built around rigorous quality standards and certifications, including ISO 13485 for medical devices, ISO 22000 for food safety systems, GMP, and QMS protocols. While the publicly available sources mention ISO 9001 and GMP specifically, it aligns with the client’s stated certifications and quality culture.
Bioptik integrates precision automation into its assembly workflows, deploying automated modules to place sensors and microchips, alongside inline calibration and testing units. This setup enables devices such as blood glucose meters to consistently meet performance requirements (e.g., ISO 15197 accuracy thresholds), while speeding up testing and facilitating smoother regulatory submissions.
Over the years, Bioptik has evolved from producing single‑function glucometers to advanced multi‑parameter systems(https://www.bioptik.com.tw/en/products/MultiFunctionalMedicalDiagnosticDevices/). Its lineup now includes compact diagnostic devices capable of testing glucose, uric acid, hemoglobin, cholesterol, triglycerides, and ketones, demonstrating its growing R&D capability and commitment to product innovation.
Bioptik’s long history, multi-site infrastructure, and systematic production protocols position it as a reliable, quality-focused partner in medical diagnostics capable of delivering precise and compliant products to global markets.
All facilities are built around rigorous quality standards and certifications, including ISO 13485 for medical devices, ISO 22000 for food safety systems, GMP, and QMS protocols. While the publicly available sources mention ISO 9001 and GMP specifically, it aligns with the client’s stated certifications and quality culture.
Bioptik integrates precision automation into its assembly workflows, deploying automated modules to place sensors and microchips, alongside inline calibration and testing units. This setup enables devices such as blood glucose meters to consistently meet performance requirements (e.g., ISO 15197 accuracy thresholds), while speeding up testing and facilitating smoother regulatory submissions.
Over the years, Bioptik has evolved from producing single‑function glucometers to advanced multi‑parameter systems(https://www.bioptik.com.tw/en/products/MultiFunctionalMedicalDiagnosticDevices/). Its lineup now includes compact diagnostic devices capable of testing glucose, uric acid, hemoglobin, cholesterol, triglycerides, and ketones, demonstrating its growing R&D capability and commitment to product innovation.
Bioptik’s long history, multi-site infrastructure, and systematic production protocols position it as a reliable, quality-focused partner in medical diagnostics capable of delivering precise and compliant products to global markets.